|

What Are Piles? What Causes Piles?
Piles are hemorrhoids that become inflamed. Hemorrhoids are masses, clumps, cushions of tissue in the anal canal - they are full of blood vessels, support tissue, muscle and elastic fibers. Although hemorrhoids are thought of as unpleasant inflammations, we all have them. It is when the hemorrhoidal cushions become too big (inflamed) that people have problems - when this happens they are called piles or pathological hemorrhoids. Put simply, "piles" are the swollen ones that cause pain and problems, hemorrhoids can refer to the swollen ones (pathological hemorrhoids) or just the normal structure. However, in most cases these days, piles and hemorrhoids have virtually the same meaning.
Piles can be of various sizes and can be internal ones (inside the anus) or external ones (outside the anus). Typically, internal piles occur from 2 to 4cm above the opening of the anus. External piles (perianal hematoma) occur on the outside edge of the anus. The internal ones are much more common.
According to the National Institutes of Health (NIH), USA, symptomatic hemorrhoids affect at least half the US population at some time in their lives, and approximately 5% of all adults have piles at any given time.
According to the National Health Service (NHS, UK), piles affect between 4% to 25% of the UK adult population. They are more common among adults aged between 45 and 65 years, as well as pregnant females.
Males and females are equally susceptible to developing hemorrhoids.
In the vast majority of cases, piles are effectively treated with OTC medications, a good fluid intake, and by following a diet high in fiber. In severe cases the piles may have to be surgically removed. Approximately 10% of patients who go and see their doctor about piles eventually have to undergo surgery.
According to Medilexicon's medical dictionary:
Hemorrhoids are "A varicose condition of the external hemorrhoidal veins causing painful swellings at the anus."
Internal Hemorrhoids are "Dilated veins beneath the mucous membrane within the sphincter."
External Hemorrhoids are "dilated veins forming tumors at the outer side of the external sphincter."
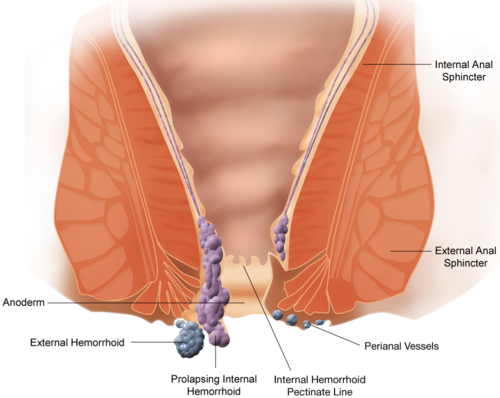
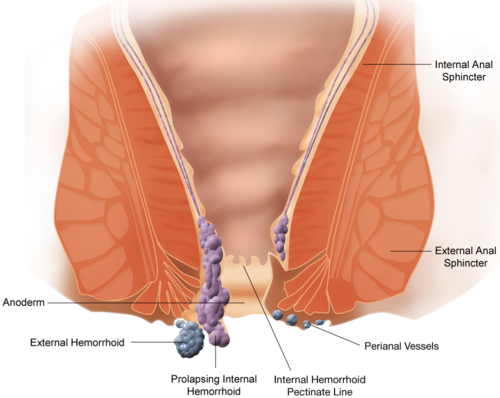
Schematic demonstrating the anatomy of hemorrhoids
What are the signs and symptoms of piles?
A symptom is something the patient feels and describes, such as a pain, while a sign is something everybody can see, such as a rash.
In most cases piles are not serious and go away on their own after a few days. In fact, a considerable number of people with hemorrhoids do not experience any symptoms and do not even know they have them.
An individual with piles may experience the following symptoms:
-
A hard lump may be felt around the anus. It consists of coagulated blood, called a thrombosed external hemorrhoid. This can be extremely painful
-
After going to the toilet, a feeling that the bowels are still full
-
Bright red blood when doing a bowel movement
-
Itchiness in the anus area
-
Mucus discharge when emptying the bowels
-
Pain while defecating
-
The anus area may be red and sore
-
When passing a stool the person may strain excessively
Internal hemorrhoids - they are classified into four grades:
-
Grade 1 - there are small inflammations, usually inside the lining of the anus. They are not visible.
-
Grade 2 - larger than Grade 1 hemorrhoids, and also inside the anus. When passing a stool they may get pushed out, but soon return.
-
Grade 3 - often called 'prolapsed hemorrhoids'; these appear outside the anus. The patient may feel them hanging out. They can be pushed back in if the patient presses with his/her finger.
-
Grade 4 - these cannot be pushed back in and need to be treated by a doctor. They are large and stay outside the anus all the time.
External hemorrhoids - called perianal hematoma. These are small lumps that are located on the outside edge of the anus. They are extremely itchy and can be painful if a blood clot forms inside (thrombosed external hemorrhoid). Thrombosed external hemorrhoid requires medical treatment straight away.
Why do piles occur?
The blood vessels around the anus and in the rectum will stretch under pressure and may swell or bulge. Inflamed veins (hemorrhoids) can develop when pressure increases in the lower rectum. This may be due to:
-
Anal intercourse
-
Chronic constipation
-
Chronic diarrhea
-
Lifting heavy weights regularly
-
Obesity/overweight
-
Pregnancy
-
Sitting on the toilet for too long
-
Straining when passing a stool
The tendency to develop hemorrhoids may also be inherited.
The risk of developing piles also grows with age.
Diagnosing piles
A qualified doctor can usually diagnose piles fairly rapidly after carrying out a physical examination. He/she will examine the patient's anus for swollen veins.
The doctor may ask the following questions:
-
Do any close relatives (parents, siblings) have piles?
-
Has there been any blood on the stools?
-
Has there been any mucus on the stools?
-
Has there been any recent weight loss?
-
Have bowel movements changed recently?
-
What color are the stools?
Internal hemorrhoids - the doctor may perform a DRE (digital rectal exam). The doctor may use a proctoscope - a hollow tube fitted with a light. The proctoscope allows the doctor to see the anal canal and take a small tissue sample from inside the rectum, which can be sent to the lab for analysis.
If the physician is presented with signs and symptoms which may suggest another digestive system disease, risk factors for colorectal cancer, and some other factors, he/she may recommend ordering an examination of the colon using colonoscopy.
What are the treatment options for piles?
In the majority of cases, piles resolve on their own without the need for any treatment. Treatments can help significantly reduce the discomfort and itching that many patients experience.
A good doctor will initially recommend some lifestyle changes.
Diet - piles can be caused by too much straining when doing bowel movements, which is the result of constipation. A change in diet can help keep the stools regular and soft. This involves eating more fiber, such as fruit and vegetables, or even switching your cereal breakfast to bran.
Water is the best drink, and the patient may be advised to increase his/her water consumption. Some experts say too much caffeine is not good.
Body weight - if the patient is obese, losing weight may help reduce the incidence and severity of hemorrhoids.
Simple things you can do yourself:
-
Try not to strain when you go to the toilet
-
Use moist toilet paper instead of dry
-
Rather than rubbing the anus area when cleaning after going to the toilet, pat instead to avoid irritation if you already have piles
Ointments, creams, pads and other OTC medications - there are some over-the-counter (OTC) medications which help soothe the redness and swelling around the anus area. Some of them contain witch hazel, hydrocortisone, or some other active ingredient which can relieve symptoms of itching and pain.
It is important to remember that they do not cure piles, they only treat the symptoms. Do not use them for more than seven consecutive days - longer periods may irritate the anus area and cause skin thinning. Unless advised to by your doctor, do not use two or more medications simultaneously.
Corticosteroids - these can reduce inflammation. However, usage must not exceed about six to seven days.
Painkillers - ask your pharmacist for suitable painkilling medications, such as acetaminophen (Tylenol, paracetamol).
Laxatives - the doctor may prescribe one if the patient suffers from constipation.
Banding - the doctor places an elastic band around the base of the pile inside the anus, cutting its blood supply. After a few days the hemorrhoids fall off. This can work for Grades 2 and 3 hemorrhoids.
Sclerotherapy - a medicine is injected into the vein to make the hemorrhoid shrink - the hemorrhoid eventually shrivels up. This is effective for Grades 2 and 3 hemorrhoids, and is a useful alternative to banding.
Infrared coagulation - also referred to as infrared light coagulation. Used for Grades 1 or 2 hemorrhoids. A device burns the hemorrhoid tissue.
Surgery - used for particularly large piles, or Grades 3 or 4 hemorrhoids. Generally, surgery is used if other procedures were not effective. Sometimes surgery is done on an outpatient basis - the patient goes home after the procedure, or he/she may have to spend the night in hospital.
-
Hemorrhoidectomy - the excess tissue that is causing the bleeding is surgically removed. This can be done in various ways. It may involve a combination of a local anesthetic and sedation, a spinal anesthetic, or a general anesthetic. This type of surgery is the most effective in completely removing piles, but there is a risk of complications, which can include difficulties passing stools, as well as urinary tract infections.
-
Hemorrhoid stapling - blood flow is blocked to the tissue of the hemorrhoid. This procedure is usually less painful than hemorrhoidectomy. However, there is a greater risk of hemorrhoid recurrence and rectal prolapse (part of the rectum sticks out of the anus).
Complications linked to piles
Anemia - hemorrhoids can sometimes cause long-term blood loss, which may lead to anemia.
Stangulated hemorrhoid - the blood supply to an internal hemorrhoid is cut off, causing severe pain, and even gangrene (death of tissue).
|
|